The Department of Justice’s (DOJ) official watchdog late last year released a report on how to fix what it said is a systemic weakness at the Federal Bureau of Prisons (BOP): its failure to obtain full data on reimbursement claims submitted by private healthcare providers, especially claims submitted electronically.
According to the “procedural reform recommendation” report DOJ’s Inspector General (IG) Michael Horowitz filed on December 20, BOP receives “incomplete and inadequate” data on healthcare services rendered by non-governmental providers. As a result, BOP cannot verify all such claims were for necessary, non-duplicative services. And without full information, the IG report says, BOP also faces an increased risk of fraud if healthcare providers exaggerate or invent claims.
In Fiscal Year 2016, BOP spent about $1.1 billion on healthcare services, with about $311 million of that total going to outside providers. For healthcare services not provided by BOP staff, the agency enters Comprehensive Medical Services (CMS) contracts with private providers, such as hospitals, clinics, diagnostic service firms, and consulting specialists. Between the years 2011 and 2020, BOP estimates such contracts will total about $1.2 billion in payments. Overall, federal spending on inmate healthcare has climbed at an annual rate of about 24% between 2010 and 2014, the IG’s report noted.
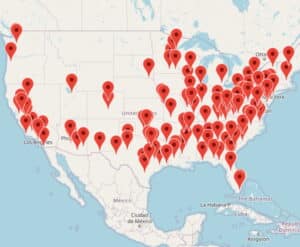
BOP has had a contract with a company — unnamed in the IG’s report — since August 2008, which was supposed to analyze and process claims from private healthcare providers. BOP’s contract with the third-party claims review contractor requires the vendor to analyze electronically submitted claims from CMS contractors. Despite that, the DOJ report said, as of February 2017 only 16 of 122 BOP prisons submitted electronic healthcare claims for review by the third-party adjudication vendor. The rest use a manual, paper-based process in which BOP staff, not the third-party vendor, review and approve claims from CMS vendors.
A 2016 revision of BOP’s contract with the third-party reviewer contained a provision, similar to one in the original 2008 contract, requiring the vendor to document its programs to detect and track intentional fraud and abuse by outside healthcare providers, and added a requirement that the vendor contact BOP immediately with a detailed report whenever its review found a “pattern of fraud and abuse.” During the nine years, the vendor has held the BOP contract, however, it never provided a single fraud report to BOP. During this time, BOP paid the adjudication review contract about $13 million, Horowitz said.
His report was harshly critical of the quality of vendor’s reviews, saying they failed to alert BOP to potentially fraudulent claims. It cited one psychiatrist who billed BOP for seeing 24 inmate patients per day, claiming 45 minutes for each session. The review vendor also approved claims for the same psychiatrist billing for as many as 61 consultations during a single day.
To remedy its current defective system, the report urged BOP to require electronic reporting, including standard codes for medical procedures performed and drugs administered, by all private healthcare providers (as is required for Medicare providers), and to ensure its third-party reviewer gets and analyzes that data, as is already required by its contract.
This article first appeared on Blogcritics.com.
Christopher Zoukis is an outspoken prisoner rights and correctional education advocate who is incarcerated at FCI Petersburg Medium in Virginia. He is an award-winning writer whose work has been published widely in major publications such as The Huffington Post, Prison Legal News, New York Daily News, and various other print and online publications. Learn more about Christopher Zoukis at christopherzoukis.com and prisoneducation.com.
Published Jan 11, 2018 by Christopher Zoukis, JD, MBA | Last Updated by Christopher Zoukis, JD, MBA on Jul 9, 2023 at 3:44 pm